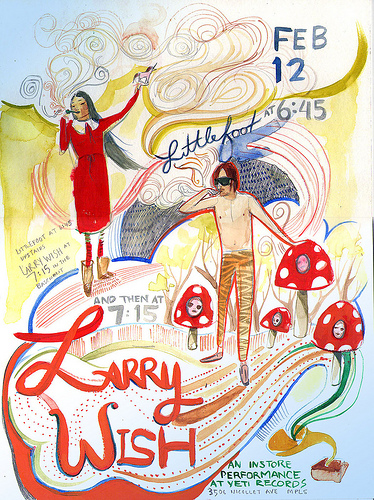
Yeti Records In Store Tonight
by josh keller · Published · Updated
Langerhans cell histiocytosis with pulmonary involvement and unilateral pneumothorax
The Turkish Journal of Pediatrics November 1, 2010 | Khanbabaee, Ghamartaj; Yeganeh, Mehrnoosh Hassas; Tabatabaei, Seyed Ahmad; Khatami, Alireza; Bazrafshan, Sholeh; Rezaei, Nima SUMMARY: Khanbabaee G, Hassas Yeganeh M, Tabatabaei SA, Khatami A, Bazrafshan S, Rezaei N. Langerhans cell histiocytosis with pulmonary involvement and unilateral pneumothorax. Turk J Pediatr 2010; 52: 638-641.
Langerhans cell histiocytosis (LCH) is a rare disorder of Langerhans cell with unknown etiology, which can uncommonly be associated with pneumothorax.
A 14-month-old female is presented here who was referred to our center due to acute respiratory distress. Reticulonodular changes with multiple cystic areas were detected in chest X-ray, whilst extensive honeycombing and cystic changes were seen in high-resolution computed tomography scan. With deterioration of respiratory distress, chest X-ray was repeated, which revealed a unilateral pneumothorax. Meanwhile, some hyperpigmented skin plaques appeared on her skull and back. The biopsy results confirmed the diagnosis of proliferative histiocytosis.
Prompt diagnosis of LCH and initiation of appropriate treatment in the patients who present with pneumothorax are vital to prevent further complications and even death in this group of patients.
Key words: histiocytic infiltration, Langerhans cell histiocytosis, pneumothorax.
Langerhans cell histiocytosis can involve several organ systems, including the lungs, bone, skin, liver, lymph nodes, pituitary gland, and thyroid. Lung involvement may occur either in isolation or as part of a multisystem disease2. Pulmonary LCH forms part of a spectrum of diseases characterized by monoclonal proliferation and infiltration of organs by Langerhans cells3. Pneumothorax (PTX) is a rare complication of pulmonary LCH in childhood4,5. However, a history of PTX in adult cases is estimated as about 10%6.
Herein, we present an infant with pulmonary LCH complicated with PTX, an unusual complication.
Case Report A 14-month-old female was admitted to the Pediatric Emergency Department of Mofid’s Children’s Hospital (Tehran, Iran) because of acute respiratory distress. She had a history of five hospitalizations in other centers with diagnoses of pneumonia. On admission, she was cyanotic and tachypneic. On physical examination, her weight was 9 kg (10-25 percentile), height 79 cm (75-90 percentile), and head circumference 46 cm (50-75 percentile). Axillary temperature was 37.6?°C, respiratory rate 68/min, heart rate 120 beats/min, and blood pressure 90/50 mmHg. Sternal and intercostal retractions and central cyanosis were found. Complete blood cell count was performed and revealed the following: white blood cells: 12,000/mm3 (polymorphonuclears: 70%, lymphocytes: 27%), red blood cells: 4.16x 106/mm3, hemoglobin: 9.2 g/dl (mean corpuscular volume [MCV]: 74.8 fl, mean corpuscular hemoglobin [MCH]: 22.1 pg, mean corpuscular hemoglobin concentration [MCHC]: 29.6 g/ dl), and platelets: 380,000/mm3. Erythrocyte sedimentation rate was 10 mm/hr. Abdominal sonography showed mild hepatomegaly and splenomegaly. Chest X-ray showed reticulonodular changes with multiple cystic areas in both lungs, with no PTX (Fig. Ia). She was transferred to the Respiratory Ward of the hospital with a suspected diagnosis of pneumonia. In high-resolution computed tomography (HRCT) scan, extensive honeycombing and cystic changes were seen in both lungs (Fig. 2) . Based on these findings in HRCT, the diagnosis of either histiocytosis or cystic fibrosis was suspected, but sweat test was normal. Bone marrow examination revealed severe erythroid hyperplasia, but no abnormal cell was seen. Bone survey was normal. Five days later, her respiratory distress suddenly deteriorated. A new chest X-ray demonstrated unilateral PTX (Fig. Ib). She was moved to the pediatric intensive care unit, and a chest tube was inserted. Meanwhile, some skin lesions similar in appearance to hyperpigmented plaques appeared on her skull and back. These lesions gradually showed some scaling (Fig. 3). The biopsy taken from these skin lesions showed histiocytic infiltration into the upper dermis, which confirmed the diagnosis of proliferative histiocytosis. Immunohistochemical evaluation revealed CD 19 positive and SlOO protein positive, which are consistent with the diagnosis of LCH. However, no lytic or sclerotic lesion was seen in the skull X-ray with normal bone density. Therefore, chemotherapy with vinblastine (6 mg/m2/week) and prednisolone (2 mg/kg/ day-maximum 60 mg/day) was started, but the patient unfortunately died in spite of the therapy. go to site langerhans cell histiocytosis site langerhans cell histiocytosis
Discussion Pneumothorax (PTX) is an unusual feature of LCH, which likely results from destruction of lung parenchyma with associated cystic changes. We described herein a case of LCH who presented with pulmonary manifestations and developed unilateral PTX and skin lesions. LCH is a rare disorder with a wide range of clinical manifestations, which presents difficulties in selecting the most effective and appropriate therapy. Due to the severity and rapid progression of disease in the infantile form of LCH, there has been even less success in determining the best treatment for this group of patients1-2.
Involvement of the lungs in LCH varies in severity, but it could lead to progressive disability and eventual death. The lungs in children are usually involved as part of a multi-system LCH, which often presents with non-specific symptoms. Although isolated organ involvement shows a relatively benign course, involvement of other organs such as liver and bone marrow should be checked, as isolated pulmonary involvement in infants is very rare. This is very important and has significant prognostic importance in LCH, while multi-system involvement associates with a high rate of mortality.
Treatment with vinblastine and etoposide in combination with one dose of corticosteroids seems to be an equally effective treatment for multi-system LCH7. However, age of less than two years and organ involvement with dysfunction are important risk factors that are associated with poor outcome8. There are no specific recommendations described for the treatment of PTX in LCH, but prompt diagnosis is an essential step in the treatment. The principle management of this complication rests on using underwater sealed drainage, whilst some patients can benefit from pleurodesis and thoracotomy9. An early consideration of extracorporeal membrane oxygenation may also have some advantages in patients whose respiratory function is deteriorating as a result of numerous PTXs4.
Early diagnosis of LCH and exact follow-up of diagnosed patients are necessary to prevent further complications. Presence of PTX (even unilateral) and skin lesions in children could alert pediatricians to suspect LCH. Appropriate management and specific chemotherapy could be started in suspected cases, even before the definite diagnosis is achieved9.
[Reference] REFERENCES 1. Weitzman S, Egeler RM. Langerhans cell histiocytosis: update for the pediatrician. Curr Opin Pediatr 2008; 20: 23-29.
2. Howarth DM, Gilchrist GS, Mullan BP, et al. Langerhans cell histiocytosis: diagnosis, natural history, management, and outcome. Cancer 1999; 85: 2278-2290.
3. Nezelof C, Basset F. Langerhans cell histiocytosis research: past, present, and future. Hematol Oncol Clin North Am 1998; 12: 385-406.
4. Yule SM, Hamilton JR, Windebank KP Recurrent pneumomediastinum and pneumothorax in Langerhans cell histiocytosis. Med Pediatr Oncol 1997; 29: 139-142.
5. Vassallo R, Ryu JH, Schroeder DR, et al. Clinical outcomes of pulmonary Langerhans’-cell histiocytosis in adults. N Engl J Med 2002; 346: 484-490.
6. Braier J, Latella A, Balancini B, et al. Isolated pulmonary Langerhans cell histiocytosis presenting with recurrent pneumothorax. Pediatr Blood Cancer 2007; 48: 241244.
7. Gadner H, Grois N, Arico M, et al; Histiocyte Society.
A randomized trial of treatment for multisystem Langerhans’ cell histiocytosis. J Pediatr 2001; 138: 728-734.
8. Nezelof C, Frileuz-Herbert F, Cronier-Sachot J. Disseminated histiocytosis X: analysis of prognostic factors based on a retrospective study of 50 cases. Cancer 1979; 44: 1824-1838.
9. Gunes T, Koklu E, Ozturk MA, et al. A case of Langerhans cell histiocytosis presented with pneumothorax. J Pediatr Hematol Oncol 2007; 29: 60-62.
[Author Affiliation] Ghamartaj Khanbabaee1, Mehrnoosh Hassas Yeganeh1, Seyed Ahmad Tabatabaei1, Alireza Khatami2, Sholeh Bazrafshan1, Nima Rezaei3-4 Departments of iPediatric Respiratory Diseases and 2Radiology, Mof?¬d Children’s Hospital, Shahid Beheshti Medical University, and 3Research Group for Immunodeficiencies, Pediatrics Center of Excellence, Children’s Medical Center, and 4Molecular Immunology Research Center and Department of Immunology, School of Medicine, Tehran University of Medical Sciences, Tehran, Iran Khanbabaee, Ghamartaj; Yeganeh, Mehrnoosh Hassas; Tabatabaei, Seyed Ahmad; Khatami, Alireza; Bazrafshan, Sholeh; Rezaei, Nima